Scientists have announced the development of “living bioelectronics,” a revolutionary technology that could transform medical diagnostics and treatment.
The innovative approach combines living cells with electronic components to create devices capable of sensing and healing skin. The breakthrough, funded partly by the U.S. Army Research Office and spearheaded by researchers from the University of Chicago, represents a significant leap forward in integrating biology and electronics.
“This is a bridge from traditional bioelectronics, which incorporates living cells as part of the therapy,” Dr. Jiuyun Shi, co-author of the study and a former PhD student in Dr. Bozhi Tian’s lab at the University of Chicago, said in a press release.
The researchers, who published their findings in the journal Science, say they have been working for over a decade to achieve this milestone in living bioelectronics.
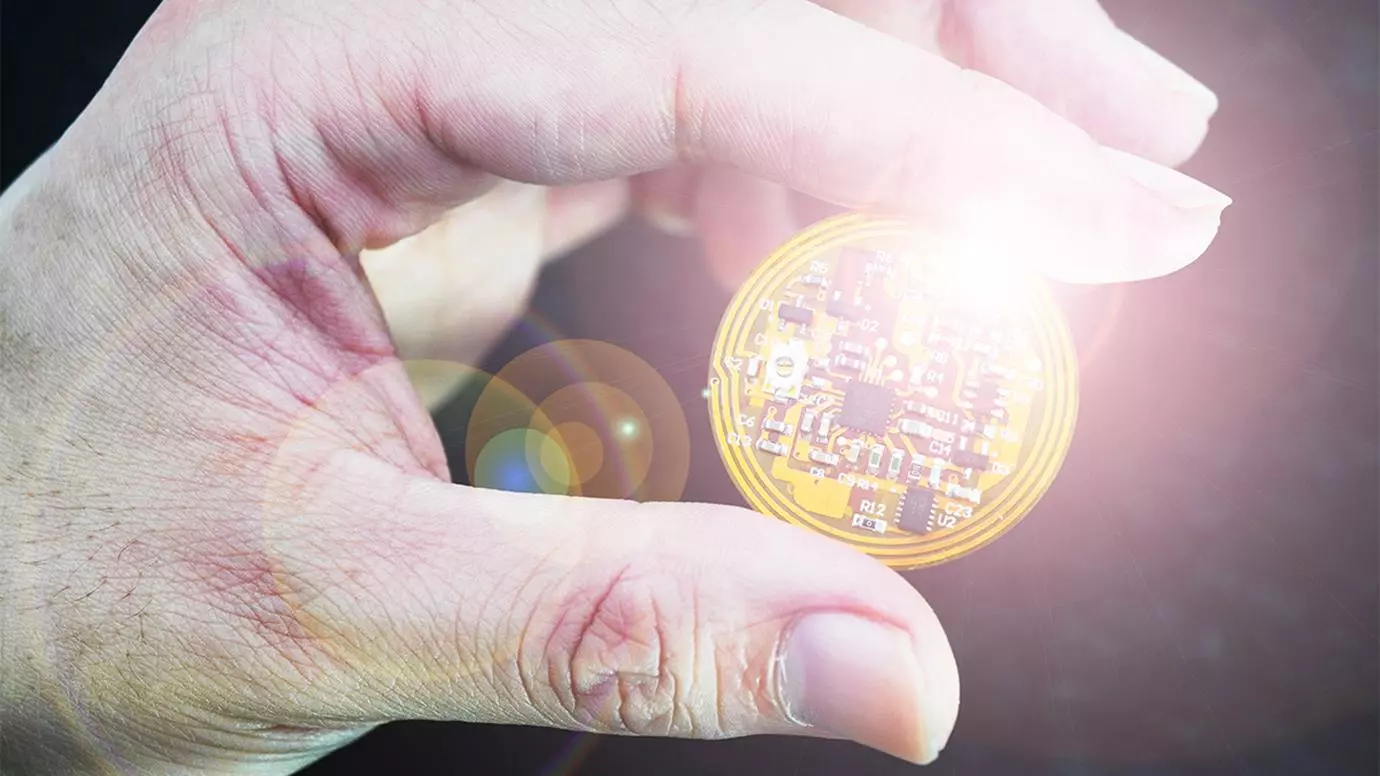
The new prototype, dubbed the “Active Biointegrated Living Electronics” or “ABLE” platform, integrates sensors, bacterial cells, and a hydrogel composite to create a seamless interface between electronic devices and biological tissues. This combination monitors and actively heals skin conditions such as psoriasis.


While transformative, the development of bioelectronics has often faced challenges due to the mechanical and biological disparities between synthetic materials and living tissues.
Bioelectronic devices like pacemakers and cochlear implants have revolutionized healthcare, saving and transforming lives. However, this integration of technology and biology carries risks. The body’s immune system may react to these devices as foreign objects, leading to rejection or other complications.
The Tian lab at the University of Chicago has long been focused on overcoming these issues by exploring how living cells and tissues interact with synthetic materials.
In previous research, the Tian Research Group developed a tiny pacemaker that is controllable by light and solid yet flexible enough to serve as bone implants. Their new approach with the ABLE platform adds a third component: living cells. The team used Staphylococcus epidermidis, a bacterium naturally found on human skin known for its anti-inflammatory properties.
The ABLE device comprises a flexible electronic circuit with embedded sensors overlaid with a gel made from tapioca starch and gelatin. This gel, designed to mimic the properties of living tissue, houses the S. epidermidis bacteria.
When applied to the skin, the bacteria secrete compounds that reduce inflammation while the sensors monitor various skin signals, such as temperature and humidity.
Tests on mice with psoriasis-like conditions demonstrated significant symptom reduction over a week-long period. With further development, the researchers believe that the device could be effective for up to six months or more. The device can be conveniently freeze-dried for storage and rehydrated when needed, making it a practical solution for long-term treatment.
“It’s like a living drug—you don’t have to refill it,” said Saehyun Kim, study co-author and PhD student in Tian’s lab.
The potential applications of the ABLE platform extend far beyond treating psoriasis. The researchers envision using this technology to accelerate wound healing in diabetic patients or developing devices that produce insulin or interface with neurons for neurological applications.
“For example, could you create an insulin-producing device or a device that interfaces with neurons?” Dr. Tian added. “There are many potential applications.”
This pioneering development in living bioelectronics builds on over a decade of research into how cells interface with materials and the chemistry and physics of hydrogels.
In a press release by the University of Chicago, Dr. Tian explained his journey to developing viable living bioelectronic technologies began 15 years ago as a postdoctoral researcher experimenting with “cyborg tissues.”
“Since then, we’ve learned so much about the fundamental questions, such as how cells interface with materials and the chemistry and physics of hydrogels, which allows us to make this leap,” he said. “To see it become [a]reality has been wonderful.”


(Image Source: University of Chicago, Jiuyun Shi and Bozhi Tian)
The advancement of ABLE is part of a broader trend in bioelectronics, which has seen several notable breakthroughs in recent years.
For instance, researchers from Northwestern University have developed a new “magic” bandage that has shown the ability to heal wounds rapidly by harvesting electricity out of thin air. Another team created neural interfaces that can translate brain signals into commands for prosthetic limbs, offering new hope for amputees and those with spinal cord injuries.
However, the integration of living cells into bioelectronic devices marks a particularly significant development, as it opens up new possibilities for treatments that are not only effective but also biocompatible and self-sustaining.
As research continues, the seamless integration of living bioelectronics has the potential to become a cornerstone of personalized and regenerative medicine, offering new hope for patients worldwide.
Dr. Tian’s research team is optimistic about the future applications of their technology, from wound healing and diabetes management to neural stimulation and beyond. The group has partnered with the Polsky Center for Entrepreneurship and Innovation to commercialize the ABLE technology, potentially bringing it to market and into the hands of healthcare providers.
“My passion has always been to push the boundaries of what is possible in science,” said Dr. Shi. “I hope our work could inspire the next generation of electronic designs.”
Tim McMillan is a retired law enforcement executive, investigative reporter and co-founder of The Debrief. His writing typically focuses on defense, national security, the Intelligence Community and topics related to psychology. You can follow Tim on Twitter: @LtTimMcMillan. Tim can be reached by email: tim@thedebrief.org or through encrypted email: LtTimMcMillan@protonmail.com