Neuroscientists have made a major discovery about the “Placebo Effect,” shedding light on a “pain control pathway” and the intricate neural mechanisms that underlie this complex and mysterious phenomenon.
The study, published in Nature, highlights a specific pain control pathway that links the cingulate cortex, pons, and cerebellum, providing new insights into how the brain processes pain relief expectations.
The placebo effect is a phenomenon where individuals experience real improvement in their symptoms or conditions after receiving a fake or inactive treatment, known as a placebo. Most researchers think the effect is influenced by psychological factors, such as expectations and the interaction between the patient and physician. While the placebo effect does impact one’s physical health, the underlying mechanisms remain poorly understood.
Now, a team from the University of North Carolina School of Medicine used a combination of cutting-edge techniques, including genetic tagging of neurons, imaging of calcium in neurons, single-cell RNA sequencing, electrophysiological recordings, and optogenetics to study the intricate neurobiology of the placebo effect down to the level of brain circuits, neurons, and synapses.
Using mice, the research team found that when they expected pain relief, specific neurons and synapses along the identified pathway were highly activated, leading to actual pain relief even without medication. This activation was linked to the rostral anterior cingulate cortex (rACC), which projects signals to the pontine nucleus (Pn) and the cerebellum. This pathway, previously not associated with pain or pain relief, was found to contain an abundance of opioid receptors, suggesting a crucial role in pain modulation.
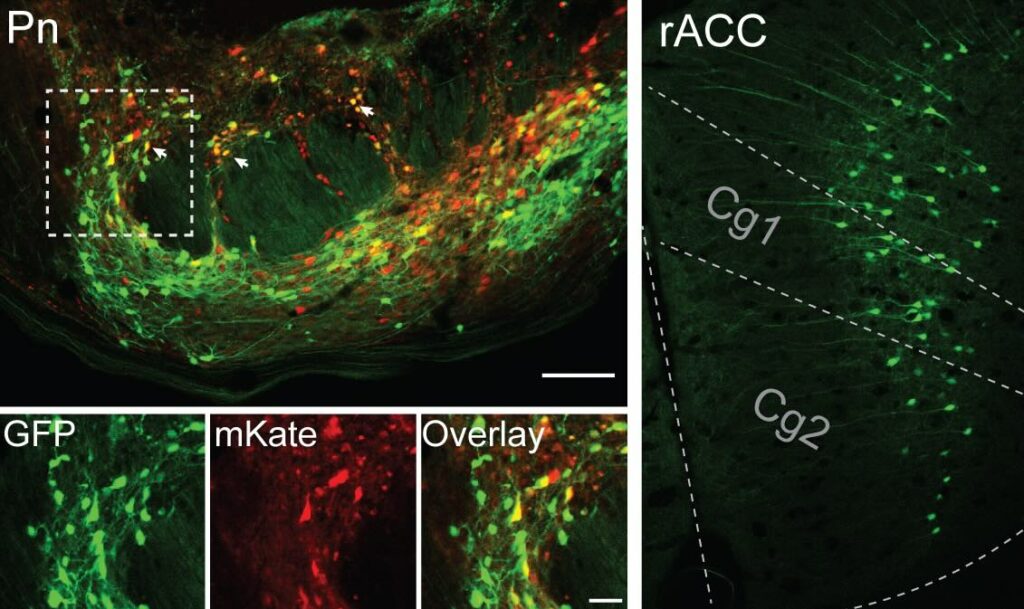
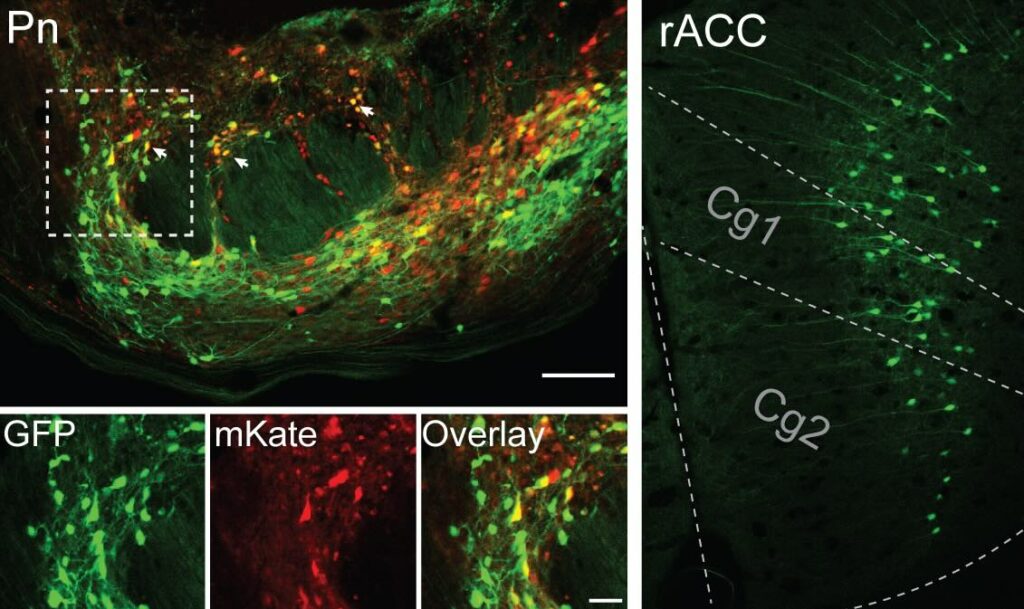
To confirm their findings, the team flipped the experiment around, and inhibited this pain control pathway. The mice experienced disrupted placebo analgesia and decreased pain thresholds. In simple terms, the placebo effect didn’t work, and the mice experienced the expected level of discomfort and pain. When the researchers re-activated this pathway, the mice experienced the pain relief without the need for a placebo.
According to the results, the “on/off” of this specific pathway suggests that the pathway is directly involved in modulating pain perception and that activating it can lead to pain relief, even in the absence of an actual pain-relieving treatment.
“That neurons in our cerebral cortex communicate with the pons and cerebellum to adjust pain thresholds based on our expectations is both completely unexpected, given our previous understanding of the pain circuitry, and incredibly exciting,” stated lead author Greg Scherrer in a statement to the press. “Our results do open the possibility of activating this pathway through other therapeutic means, such as drugs or neurostimulation methods to treat pain.”
The study’s findings have some serious implications for understanding the biological basis of the placebo effect and its potential applications in pain management.
The placebo effect has long been recognized as a powerful force in medicine, with numerous studies demonstrating its impact on various clinical and physiological outcomes. However, the underlying neural mechanisms have remained a mystery. The study authors believe that their work provides a crucial step forward in better understanding these mechanisms, highlighting the complex interplay between brain regions and neurochemical mediators involved in placebo pain relief.
The team hopes that the discovery of this pain control pathway can be leveraged to develop more effective treatments for chronic pain and related disorders, which have proven challenging to manage with traditional therapeutic approaches.
“We all know we need better ways to treat chronic pain, particularly treatments without harmful side effects and addictive properties,” Scherrer explained. “We think our findings open the door to targeting this novel neural pain pathway to treat people in a different but potentially more effective way.”
MJ Banias covers space, security, and technology with The Debrief. You can email him at mj@thedebrief.org or follow him on Twitter @mjbanias.